
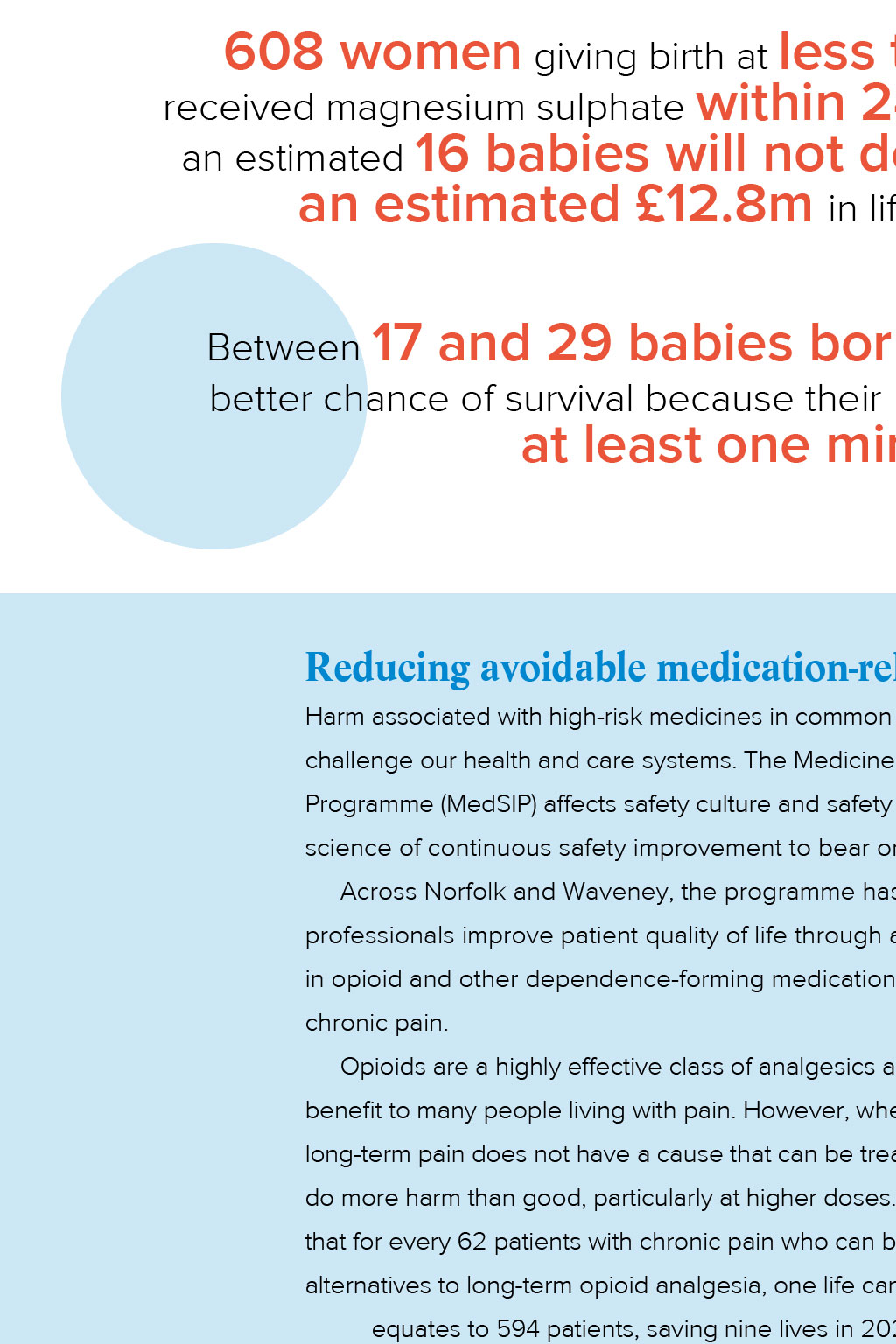

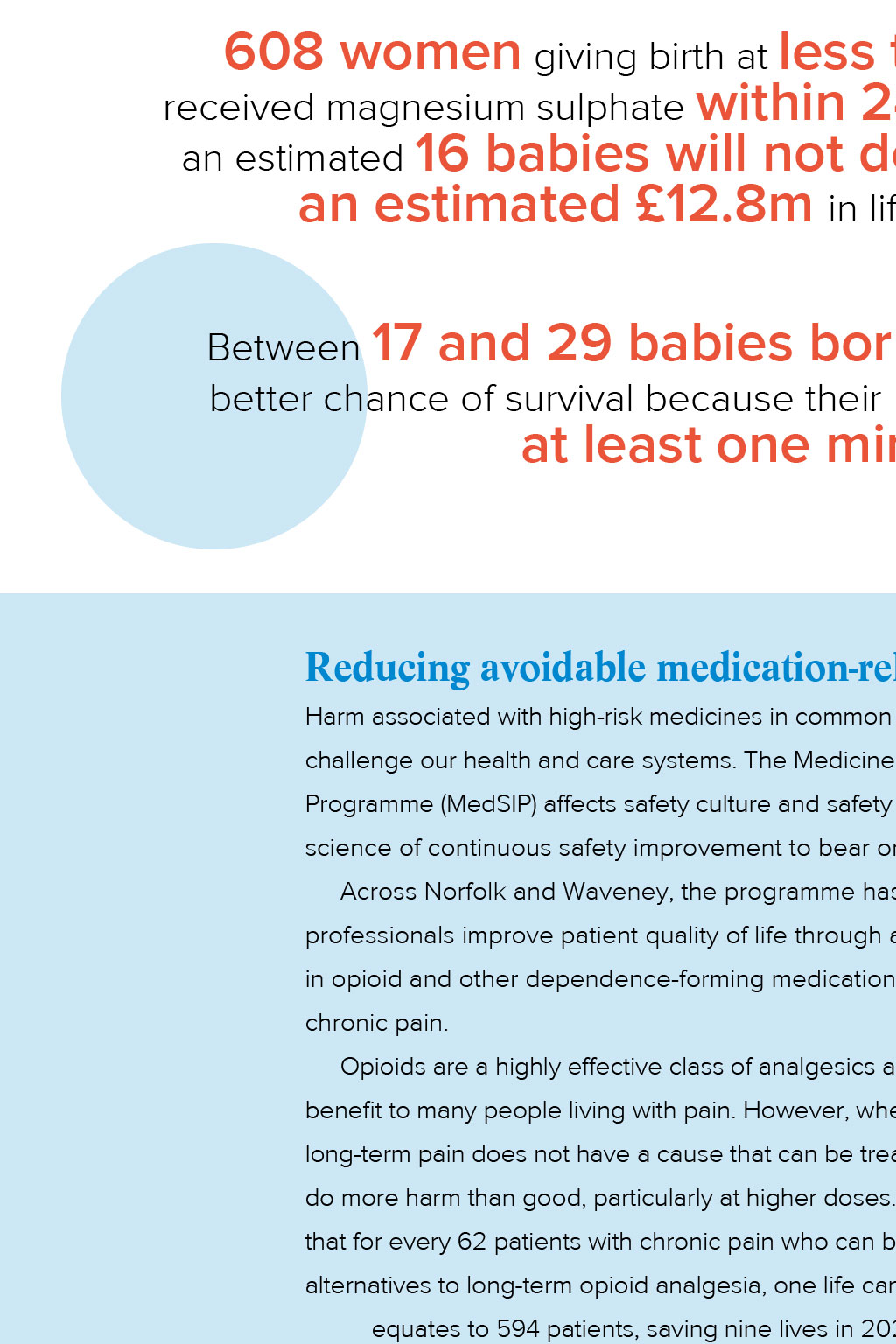
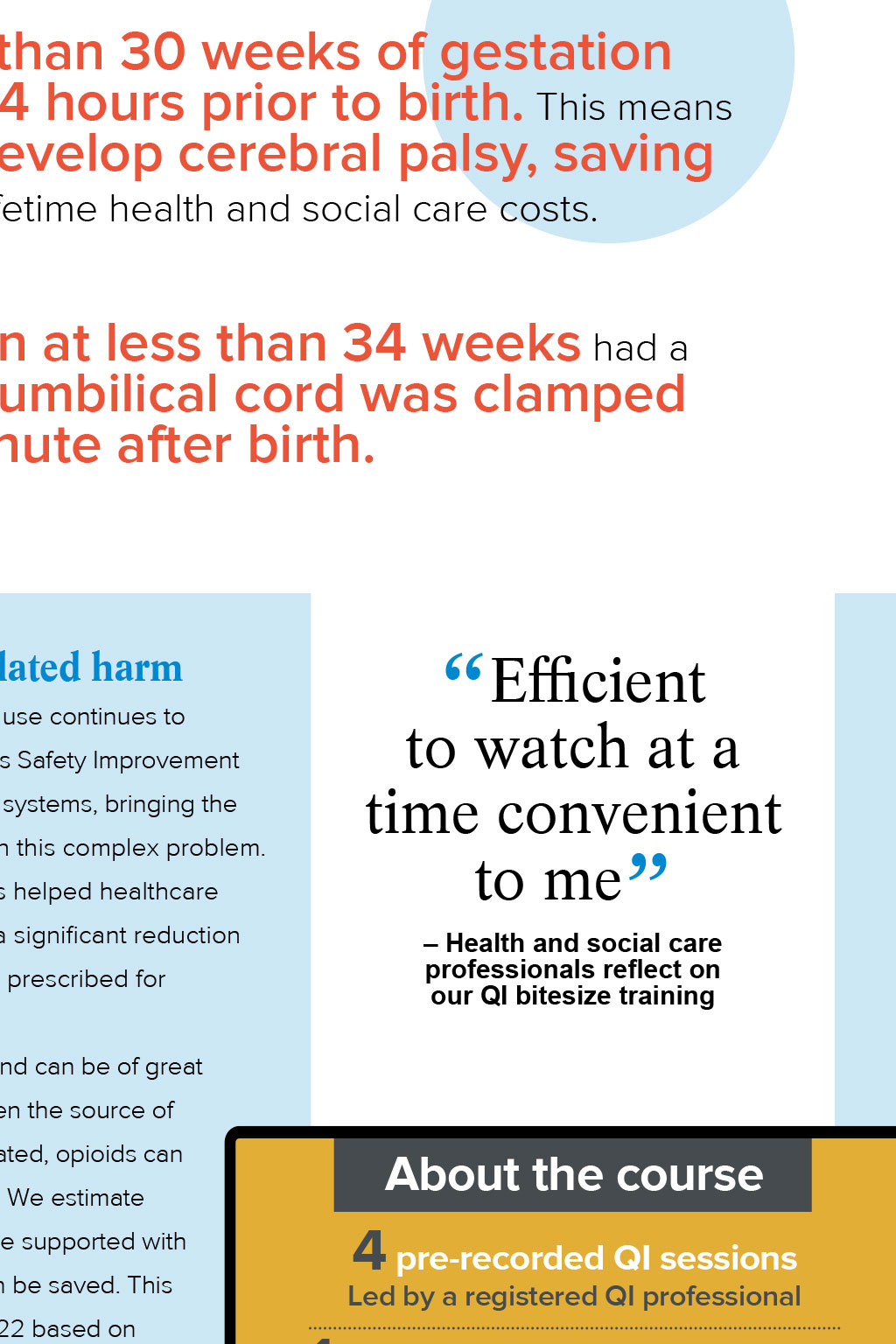
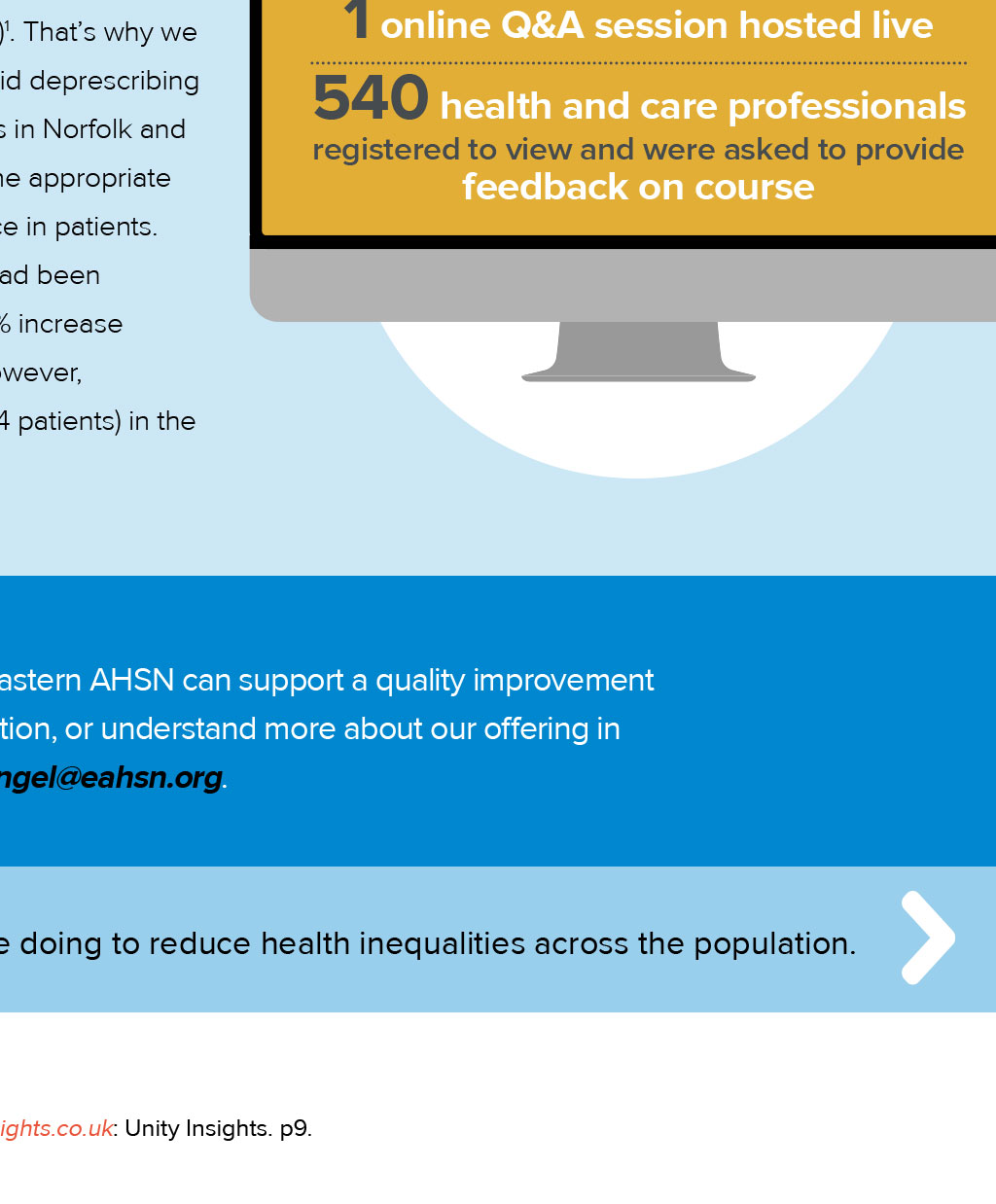

Embedding system-wide patient safety improvement Improvement and innovation should never come at the price of patient safety. Caroline Angel, Director of Patient Safety at Eastern AHSN, shares how we have worked across acute, non-acute and community settings to share and spread evidencebased practices, products and tools. A s health and care professionals, we all want to follow best practice in how we deliver services, giving our patients the chance to achieve the best outcomes, while reducing the risk of anything going wrong. The safety of patients is a critical thread running through all of Eastern AHSNs work, but we have specific programmes aimed at helping services in our region improve their processes and practice. The National Patient Safety Improvement Programmes (NatPatSIPs) support a culture of safety, continuous learning and sustainable improvement across organisational boundaries throughout the healthcare system. They are delivered by Patient Safety Collaboratives (PSCs), which are hosted by AHSNs. This year, we have worked with trusts and commissioners across the East of England on five core programmes. Patient safety at a system level Joy Kirby, assistant director clinical quality, patient safety specialist, NHS England East of England Patient safety and quality improvement are central to NHS services, and while its always been a priority, integrated care systems (ICSs) present an invaluable opportunity to implement NHS Englands National Patient Safety Strategy across the region. We have been working closely with colleagues from Eastern AHSN and patient safety specialists within ICSs to deliver the strategy and embed the Patient Safety Incident Response Framework (PSIRF) to continuously improve patient safety, building on the foundations of a safer culture and safer systems. This is a huge piece of work across England, and Eastern AHSN colleagues have been instrumental in convening healthcare professionals from across organisations The teams expertise and commitment have been instrumental in strengthening the patientsafety culture across the East of England to facilitate the sharing of best practice in the implementation and embedding of PSIRF to ensure safe and effective patient care. Identifying deterioration to avoid hospitalisation We have continued to work with care homes to adopt a common language related to deterioration across the health and social care system, to ensure clarity when transferring vital clinical information between healthcare professionals. We supported a pilot to combine this with a remote-monitoring tool, which led to a reduction of 73 (15.75%) conveyances to hospital, with an estimated cost saving of 201,810 over six months across 33 care homes. As of March 2023, 78% of care homes have spread the use of deterioration managment tools in place to all residents and 22% are testing or implementing deterioration management tools. Having established a Care Home Network to convene care staff and support this work, we have handed over management of the group to the Regional Enhanced Health in Care Homes (EHCH) lead upon closure of this programme from April 2023 onwards. A stronger start in life We have worked with maternity units across the region to improve the outcomes of very premature infants through the Maternity and Neonatal Safety Improvement Programme (MatNeoSIP). Our work included supporting the spread and adoption of the preterm perinatal optimisation care pathway, which aims to reduce stillbirths, neonatal deaths and hypoxic brain injury. In our region, our continued support through this programme has meant that 608 women giving birth at less than 30 weeks of gestation received magnesium sulphate within 24 hours prior to birth. This means an estimated 16 babies will not develop cerebral palsy, saving an estimated 12.8m in lifetime health and social care costs. Between 17 and 29 babies born at less than 34 weeks had a better chance of survival because their umbilical cord was clamped at least one minute after birth. Reducing avoidable medication-related harm Efficient to watch at a time convenient to me Harm associated with high-risk medicines in common use continues to challenge our health and care systems. The Medicines Safety Improvement Programme (MedSIP) affects safety culture and safety systems, bringing the science of continuous safety improvement to bear on this complex problem. Across Norfolk and Waveney, the programme has helped healthcare professionals improve patient quality of life through a significant reduction Health and social care professionals reflect on our QI bitesize training in opioid and other dependence-forming medication prescribed for chronic pain. Opioids are a highly effective class of analgesics and can be of great benefit to many people living with pain. However, when the source of long-term pain does not have a cause that can be treated, opioids can About the course do more harm than good, particularly at higher doses. We estimate 4 pre-recorded QI sessions that for every 62 patients with chronic pain who can be supported with alternatives to long-term opioid analgesia, one life can be saved. This equates to 594 patients, saving nine lives in 2022 based on data from Unity Insights (December 2022) . Thats why we 1 Our online quality improvement bitesize learning sessions have been watched more than 650 times. Find out more on our website have supported the rollout of the opioid deprescribing toolkit across primary care providers in Norfolk and Waveney, to enable them to use the appropriate Led by a registered QI professional needed 1 onlineHR Q&Apic session hosted live 540 health and care professionals registered to view and were asked to provide tools to help reduce opioid reliance in patients. feedback on course Since 2018, prescribing rates had been increasing year on year, with an 11% increase (2,262 patients) by March 2022. However, prescribing has reduced by 2.6% (594 patients) in the nine months to December 2022. Share this article If you want to discuss how Eastern AHSN can support a quality improvement programme in your organisation, or understand more about our offering in 2023/24, contact caroline.angel@eahsn.org. Return to About Us Up next: Read what were doing to reduce health inequalities across the population. References 1 Medications Safety Improvement Programme (MedSIP) Methodology Report. unityinsights.co.uk: Unity Insights. p9.